Brian Najarian and Jeffrey Lawton
DEFINITION
![]() Proximal interphalangeal (PIP) joint fracture-dislocations are intra-articular injuries that include a concomitant soft tissue injury to the surrounding capsular and ligamentous structures.
Proximal interphalangeal (PIP) joint fracture-dislocations are intra-articular injuries that include a concomitant soft tissue injury to the surrounding capsular and ligamentous structures.
![]() The injury can result from axial, bending, and torsional loads, or combinations thereof.
The injury can result from axial, bending, and torsional loads, or combinations thereof.
![]() These injuries of the finger are relatively common and potentially disabling, and may result in:
These injuries of the finger are relatively common and potentially disabling, and may result in:
![]() Joint stiffness
Joint stiffness
![]() Persistent subluxation
Persistent subluxation
![]() Posttraumatic arthritis
Posttraumatic arthritis
![]() Chronic pain
Chronic pain
![]() Stability and alignment are more important goals than articular congruency in determining a successful outcome.18
Stability and alignment are more important goals than articular congruency in determining a successful outcome.18
![]() Evaluation and treatment may be delayed, with the injury dismissed as a “jammed finger.”
Evaluation and treatment may be delayed, with the injury dismissed as a “jammed finger.”
ANATOMY
![]() The PIP joint is a hinge joint, consisting of radial and ulnar condyles on the proximal phalanx, with matching concavities on the middle phalangeal base. This construction allows for a wide range of motion (ROM) in flexion and extension, but relative rigidity in abduction and adduction.
The PIP joint is a hinge joint, consisting of radial and ulnar condyles on the proximal phalanx, with matching concavities on the middle phalangeal base. This construction allows for a wide range of motion (ROM) in flexion and extension, but relative rigidity in abduction and adduction.
![]() The PIP joint has an arc of motion of 120 degrees and accounts for 85% of the motion required to grasp an object.2
The PIP joint has an arc of motion of 120 degrees and accounts for 85% of the motion required to grasp an object.2
![]() The joint derives its stability from its bony articular congruence and its soft tissue restraints (FIG 1).
The joint derives its stability from its bony articular congruence and its soft tissue restraints (FIG 1).
![]() The volar plate resists dorsal stress, is taut in extension, and often fails distally from bone.
The volar plate resists dorsal stress, is taut in extension, and often fails distally from bone.
![]() Checkrein ligaments are slender proximal extensions of the volar plate under which branches of the digital arteries pass, supplying the joint and vincula and nourishing the flexor tendons.
Checkrein ligaments are slender proximal extensions of the volar plate under which branches of the digital arteries pass, supplying the joint and vincula and nourishing the flexor tendons.
![]() Collateral ligaments, the primary soft tissue restraints, have two components:
Collateral ligaments, the primary soft tissue restraints, have two components:
![]() The proper collateral ligaments (radial and ulnar), which insert on the middle phalanx, provide the principal resistance to abduction/adduction stress. These ligaments are commonly injured in dorsal dislocations. Injury to the radial collateral ligament is more common than injury to the ulnar collateral ligament by nearly six-fold.
The proper collateral ligaments (radial and ulnar), which insert on the middle phalanx, provide the principal resistance to abduction/adduction stress. These ligaments are commonly injured in dorsal dislocations. Injury to the radial collateral ligament is more common than injury to the ulnar collateral ligament by nearly six-fold.
![]() The accessory collateral ligaments arise from a conjoined origin just volar to the proper collateral ligament and insert on the volar plate.
The accessory collateral ligaments arise from a conjoined origin just volar to the proper collateral ligament and insert on the volar plate.
![]() The extensor complex limits volarly directed stress.
The extensor complex limits volarly directed stress.
![]() The central slip attaches to the dorsal tubercle on the base of the middle phalanx.
The central slip attaches to the dorsal tubercle on the base of the middle phalanx.
![]() The conjoint lateral bands run obliquely on each side of the joint.
The conjoint lateral bands run obliquely on each side of the joint.
![]() The transverse retinacular ligament connects the central slip and the conjoint lateral bands and extends laterally.
The transverse retinacular ligament connects the central slip and the conjoint lateral bands and extends laterally.
![]() For a dislocation to occur, at least one, often two, and sometimes all three of these structures must be significantly disrupted.
For a dislocation to occur, at least one, often two, and sometimes all three of these structures must be significantly disrupted.
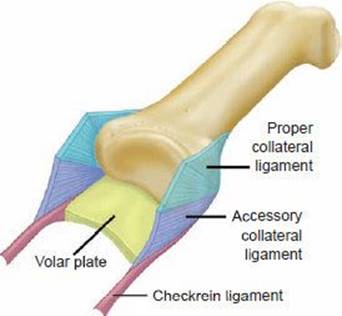
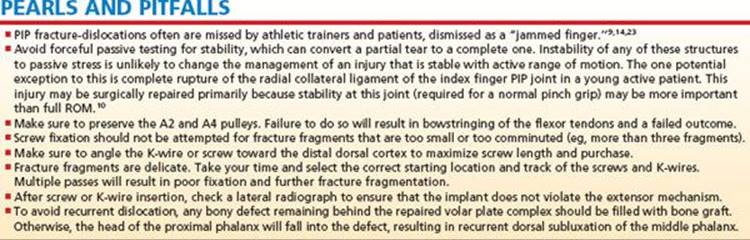
FIG 1 • Diagram of proximal interphalangeal (PIP) joint anatomy. The PIP joint is a hinge joint that derives its stability from bony articular congruence of the proximal and middle phalanx and soft tissue restraints: the volar plate and its checkrein ligament extensions, the proper and accessory collateral ligaments, and the extensor complex (not shown).
PATHOGENESIS AND CLASSIFICATION
![]() The PIP joint is uniquely susceptible to injury.
The PIP joint is uniquely susceptible to injury.
![]() The pattern of joint injury depends on the direction, degree, and rate of force application.
The pattern of joint injury depends on the direction, degree, and rate of force application.
![]() The three main groups of PIP fracture dislocations are defined by the mechanism of injury force and the direction of deformity (FIG 2).
The three main groups of PIP fracture dislocations are defined by the mechanism of injury force and the direction of deformity (FIG 2).
![]() Dorsal subluxation, or dislocation of the middle, the most common type, is caused by hyperextension and axial loading of the middle phalanx against the head of the proximal phalanx. The result is a fracture involving the base of the middle phalanx and dorsal positioning of the middle phalanx.
Dorsal subluxation, or dislocation of the middle, the most common type, is caused by hyperextension and axial loading of the middle phalanx against the head of the proximal phalanx. The result is a fracture involving the base of the middle phalanx and dorsal positioning of the middle phalanx.
This injury can be subclassified into three types based on the amount of volar middle phalanx articular surface involved, as determined on a lateral radiograph.13 The degree of instability is directly proportional to volar lip fragment size due to the loss of collateral ligament support, and the articular buttress (see FIG 3B in Chap. HA-35).
![]() Stable: less than 30% of the articular surface, reduced in extension
Stable: less than 30% of the articular surface, reduced in extension
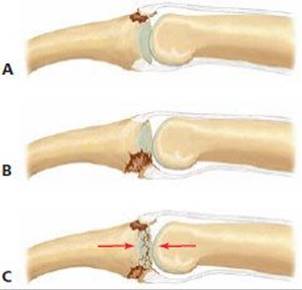
FIG 2 • PIP fracture-dislocation classifications. The three main groups of PIP fracture-dislocations are volar (A), dorsal (B), and pilon (C).
![]() Tenuous: 30% to 50% of the articular surface, reduction maintained with less than 30 degrees of flexion
Tenuous: 30% to 50% of the articular surface, reduction maintained with less than 30 degrees of flexion
![]() Unstable: either more than 50% of the articular surface or 30% to 50% of the articular surface, but requiring more than 30 degrees of flexion to maintain reduction
Unstable: either more than 50% of the articular surface or 30% to 50% of the articular surface, but requiring more than 30 degrees of flexion to maintain reduction
![]() Volar subluxation, or dislocation of the middle phalanx, is less common and is thought to be caused by forced flexion of an extended joint.
Volar subluxation, or dislocation of the middle phalanx, is less common and is thought to be caused by forced flexion of an extended joint.
![]() Stable: joint reduction in extension
Stable: joint reduction in extension
![]() Unstable: palmar subluxation of middle phalanx with the joint extended
Unstable: palmar subluxation of middle phalanx with the joint extended
![]() Pilon injuries are not associated with significant subluxation or dislocation. They are caused by an axial force on a partially flexed PIP joint, resulting in comminution of the articular surface of the middle phalanx (most commonly, volar and dorsal articular fragments surrounding a central depressed fragment)
Pilon injuries are not associated with significant subluxation or dislocation. They are caused by an axial force on a partially flexed PIP joint, resulting in comminution of the articular surface of the middle phalanx (most commonly, volar and dorsal articular fragments surrounding a central depressed fragment)
![]() Unicondylar fractures of the head of the proximal phalanx, another variant of this injury type, are included in a classification system proposed by Weiss and Hastings21 (see Chap. HA-33).
Unicondylar fractures of the head of the proximal phalanx, another variant of this injury type, are included in a classification system proposed by Weiss and Hastings21 (see Chap. HA-33).
![]() These injuries also can be accompanied by dislocation of the PIP joint and nearly always are unstable and require operative fixation. They often are amenable to the same approaches and fixation methods presented here.
These injuries also can be accompanied by dislocation of the PIP joint and nearly always are unstable and require operative fixation. They often are amenable to the same approaches and fixation methods presented here.
NATURAL HISTORY
![]() Following injury, the PIP joint quickly stiffens. Pain and instability limit motion initially; then the joint capsule and ligaments become fibrotic.
Following injury, the PIP joint quickly stiffens. Pain and instability limit motion initially; then the joint capsule and ligaments become fibrotic.
![]() Over time the unreduced PIP joint will become arthritic and painful.
Over time the unreduced PIP joint will become arthritic and painful.
HISTORY AND PHYSICAL FINDINGS
![]() Patients present following a traumatic event to the digit, frequently one that occurred some time ago.
Patients present following a traumatic event to the digit, frequently one that occurred some time ago.
![]() In the acute setting, the primary complaints are pain and swelling of the joint and digit.
In the acute setting, the primary complaints are pain and swelling of the joint and digit.
![]() Patients with subacute and chronic injuries are focused primarily on stiffness, loss of function, and persistent swelling, and secondarily on pain.
Patients with subacute and chronic injuries are focused primarily on stiffness, loss of function, and persistent swelling, and secondarily on pain.
![]() The history must include a detailed description of the mechanism of injury and any previous treatment.
The history must include a detailed description of the mechanism of injury and any previous treatment.
![]() Inspection
Inspection
![]() Evaluate the skin and soft tissues for swelling and for any open or healed wounds that could indicate an open fracturedislocation.
Evaluate the skin and soft tissues for swelling and for any open or healed wounds that could indicate an open fracturedislocation.
![]() Deformity in extension or flexion indicates whether the dislocation is volar or dorsal, respectively.
Deformity in extension or flexion indicates whether the dislocation is volar or dorsal, respectively.
![]() Axial or rotational malalignment may result from articular depression of a condyle. This can be recognized clinically as subtle angulation when full digital extension is attempted.
Axial or rotational malalignment may result from articular depression of a condyle. This can be recognized clinically as subtle angulation when full digital extension is attempted.
![]() Tenderness
Tenderness
![]() The acute location of greatest tenderness on palpation may indicate which soft tissue structures are injured.
The acute location of greatest tenderness on palpation may indicate which soft tissue structures are injured.
![]() ROM
ROM
![]() Adequate evaluation may be difficult in the acute setting due to pain. After neurologic examination, a digital block may be necessary.
Adequate evaluation may be difficult in the acute setting due to pain. After neurologic examination, a digital block may be necessary.
![]() Elson test (FIG 3)
Elson test (FIG 3)
![]() From a 90-degree flexed position over the edge of a table, ask the patient to actively extend the PIP joint of the involved finger against resistance. If the central slip is intact, the examiner will feel an extension force from the middle phalanx. In addition, the distal interphalangeal (DIP) joint remains flail during this effort, because the competent central slip prevents the lateral bands from acting distally.
From a 90-degree flexed position over the edge of a table, ask the patient to actively extend the PIP joint of the involved finger against resistance. If the central slip is intact, the examiner will feel an extension force from the middle phalanx. In addition, the distal interphalangeal (DIP) joint remains flail during this effort, because the competent central slip prevents the lateral bands from acting distally.
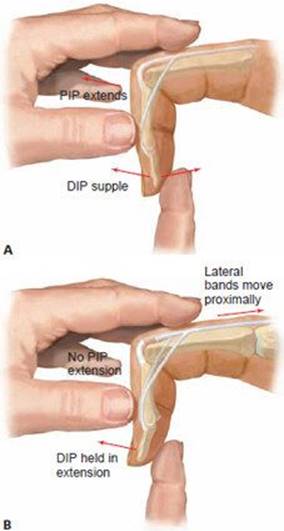
FIG 3 • Elson test. A. Intact central slip. From a 90-degree flexed position, the patient can actively extend the PIP joint of the involved finger against resistance. The distal interphalangeal (DIP) joint is supple. B. Ruptured central slip. The patient cannot actively extend the PIP joint against resistance and has fixed extension at the DIP joint, due to the extensor action of the lateral bands alone.
![]() An absence of extension force at the PIP joint and fixed extension at the DIP joint (due to the extensor action of the lateral bands alone) is diagnostic of a complete rupture of the central slip. In the acute setting, the patient may be reluctant to perform this test due to pain, but this can be relieved by proximal infiltration with local anesthetic around the dorsal sensory nerves of the digit.7
An absence of extension force at the PIP joint and fixed extension at the DIP joint (due to the extensor action of the lateral bands alone) is diagnostic of a complete rupture of the central slip. In the acute setting, the patient may be reluctant to perform this test due to pain, but this can be relieved by proximal infiltration with local anesthetic around the dorsal sensory nerves of the digit.7
![]() Note the range of motion through which the joint remains reduced. In the case of a dorsal dislocation, the degree of extension that results in instability or redislocation determines the angle for the extension block splint.
Note the range of motion through which the joint remains reduced. In the case of a dorsal dislocation, the degree of extension that results in instability or redislocation determines the angle for the extension block splint.
![]() An irreducible joint is consistent with entrapment of a soft tissue structure (eg, volar plate, collateral ligament, flexor or extensor tendon) in the joint, which usually necessitates urgent surgery.
An irreducible joint is consistent with entrapment of a soft tissue structure (eg, volar plate, collateral ligament, flexor or extensor tendon) in the joint, which usually necessitates urgent surgery.
![]() The neurovascular examination usually is normal.
The neurovascular examination usually is normal.
![]() Subjective complaints of paresthesias and objective measure of capillary refill should be noted, both preand postreduction.
Subjective complaints of paresthesias and objective measure of capillary refill should be noted, both preand postreduction.
IMAGING AND OTHER DIAGNOSTIC STUDIES
![]() Posteroanterior (PA), lateral, and partially supinated and pronated oblique radiographs of the involved digit(s) are required.
Posteroanterior (PA), lateral, and partially supinated and pronated oblique radiographs of the involved digit(s) are required.
![]() Oblique views help to identify fracture planes and determine the extent of comminution, valuable for surgical planning.
Oblique views help to identify fracture planes and determine the extent of comminution, valuable for surgical planning.
![]() It is critical to determine amount of articular involvement on a true lateral film in full PIP joint extension to evaluate stability of the joint.
It is critical to determine amount of articular involvement on a true lateral film in full PIP joint extension to evaluate stability of the joint.
![]() Radiographs can be misleading, suggesting that a very simple fracture involving only a small fragment of the bone has occurred. This fragment is potentially the major attachment of a collateral ligament, the volar plate, or a tendon. The resultant incompetence of these structures can render the joint grossly or potentially unstable (FIG 4A).
Radiographs can be misleading, suggesting that a very simple fracture involving only a small fragment of the bone has occurred. This fragment is potentially the major attachment of a collateral ligament, the volar plate, or a tendon. The resultant incompetence of these structures can render the joint grossly or potentially unstable (FIG 4A).
![]() V sign13 (FIG 4B)
V sign13 (FIG 4B)
![]() On a postreduction true lateral radiograph of the digit, divergence of the dorsal articular surfaces from the central portion of the joint creates a V-shaped gap between the articular surfaces of the head of the proximal phalanx and the undamaged portion of the middle phalanx base.
On a postreduction true lateral radiograph of the digit, divergence of the dorsal articular surfaces from the central portion of the joint creates a V-shaped gap between the articular surfaces of the head of the proximal phalanx and the undamaged portion of the middle phalanx base.
![]() The presence of this sign indicates an incompletely reduced joint.
The presence of this sign indicates an incompletely reduced joint.
![]() Dynamic fluoroscopy is extremely valuable in evaluating the reduction and its stability.
Dynamic fluoroscopy is extremely valuable in evaluating the reduction and its stability.
![]() Hinged flexion is a variant of the V sign in which congruent rotation of the joint is replaced by abnormal translation as the joint is actively flexed and extended across the flattened fracture segments.
Hinged flexion is a variant of the V sign in which congruent rotation of the joint is replaced by abnormal translation as the joint is actively flexed and extended across the flattened fracture segments.
![]() The joint position that results in instability or redislocation is best determined fluoroscopically.
The joint position that results in instability or redislocation is best determined fluoroscopically.
DIFFERENTIAL DIAGNOSIS
![]() Pure dislocation (simple or complex)
Pure dislocation (simple or complex)
![]() Extra-articular fractures
Extra-articular fractures
![]() “Jammed finger”—collateral sprain9,14,23
“Jammed finger”—collateral sprain9,14,23
![]() Volar plate injury
Volar plate injury
![]() Central slip injury
Central slip injury
NONOPERATIVE MANAGEMENT
![]() Prompt recognition of the complexity of injury and an understanding of the appropriate treatment options are essential for optimal management of these fractures.
Prompt recognition of the complexity of injury and an understanding of the appropriate treatment options are essential for optimal management of these fractures.
![]() Although fractures and dislocations of the PIP joint have the potential to be disabling, most can be treated with closed reduction, splinting, early motion, and close follow-up.
Although fractures and dislocations of the PIP joint have the potential to be disabling, most can be treated with closed reduction, splinting, early motion, and close follow-up.
![]() Closed reduction is almost always successful for acute dorsal PIP dislocations. Volar dislocations are more problematic, especially if the deformity has a rotary component.
Closed reduction is almost always successful for acute dorsal PIP dislocations. Volar dislocations are more problematic, especially if the deformity has a rotary component.
![]() Reductions performed immediately after the injury often can be accomplished without anesthesia. If reduction is delayed, a digital block with 1% lidocaine (without epinephrine) is helpful.
Reductions performed immediately after the injury often can be accomplished without anesthesia. If reduction is delayed, a digital block with 1% lidocaine (without epinephrine) is helpful.
![]() Always make sure to complete a careful neurologic examination of the digit before performing an anesthetic block. Confirm adequate anesthesia before manipulation.
Always make sure to complete a careful neurologic examination of the digit before performing an anesthetic block. Confirm adequate anesthesia before manipulation.
![]() Be gentle, and limit the number of attempts. Irreducible dislocations usually are caused by soft tissue interposition.
Be gentle, and limit the number of attempts. Irreducible dislocations usually are caused by soft tissue interposition.
![]() Dorsal dislocations can be reduced with gentle traction on the finger with the wrist in the neutral position, followed by pressing the base of the middle phalanx in a volar direction while holding the proximal phalanx steady.
Dorsal dislocations can be reduced with gentle traction on the finger with the wrist in the neutral position, followed by pressing the base of the middle phalanx in a volar direction while holding the proximal phalanx steady.
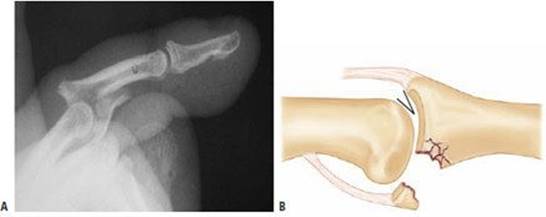
FIG 4 • A. Unstable dorsal PIP fracture-dislocation. This lateral radiograph of a typical PIP joint fracture, demonstrates dorsal dislocation of the middle phalanx on the proximal phalanx due to the large amount of volar articular surface involved (over 50%). B. The V-sign in an incompletely reduced dorsal fracture-dislocation. Divergence of the dorsal articular surfaces from the central portion of the joint creates a V-shaped gap, which can be demonstrated on a lateral radiograph.
![]() Volar dislocations without a rotatory component usually are reducible with gentle traction.
Volar dislocations without a rotatory component usually are reducible with gentle traction.
![]() Place the wrist in the neutral position and apply a dorsally directed force to the middle phalanx and a volarly directed force on the proximal phalanx.
Place the wrist in the neutral position and apply a dorsally directed force to the middle phalanx and a volarly directed force on the proximal phalanx.
![]() These dislocations, which usually can be treated with closed reduction, commonly involve an avulsion of the central slip.
These dislocations, which usually can be treated with closed reduction, commonly involve an avulsion of the central slip.
![]() Volar dislocations with a rotatory component often are difficult to reduce by closed means. The head of the proximal phalanx becomes trapped between the central slip and one of the lateral bands of the extensor mechanism.
Volar dislocations with a rotatory component often are difficult to reduce by closed means. The head of the proximal phalanx becomes trapped between the central slip and one of the lateral bands of the extensor mechanism.
![]() These injuries occasionally can be reduced closed by placing the metacarpophalangeal (MCP) and PIP joints in 90 degrees of flexion with the wrist extended, applying light traction, and rotating the middle phalanx in the direction opposite to the deformity.
These injuries occasionally can be reduced closed by placing the metacarpophalangeal (MCP) and PIP joints in 90 degrees of flexion with the wrist extended, applying light traction, and rotating the middle phalanx in the direction opposite to the deformity.
SURGICAL MANAGEMENT
![]() Surgical management is difficult for two reasons:
Surgical management is difficult for two reasons:
![]() The fracture fragments can be small and comminuted, making anatomic reduction and stabilization with implants difficult.
The fracture fragments can be small and comminuted, making anatomic reduction and stabilization with implants difficult.
![]() The need for early mobilization of the joint to prevent stiffness requires rigid fixation of these fragments.
The need for early mobilization of the joint to prevent stiffness requires rigid fixation of these fragments.
![]() These fractures have a high risk of redisplacement, and patients must be warned of the possibility that repeat surgical treatment of the fracture may be necessary.
These fractures have a high risk of redisplacement, and patients must be warned of the possibility that repeat surgical treatment of the fracture may be necessary.
![]() The specific injury and fracture pattern often dictate the most appropriate method of treatment. Some methods can be used in combination.
The specific injury and fracture pattern often dictate the most appropriate method of treatment. Some methods can be used in combination.
![]() For stable, reducible fractures, typically involving less than 30% of the articular surface, treatment includes:
For stable, reducible fractures, typically involving less than 30% of the articular surface, treatment includes:
![]() Extension block splinting and pinning
Extension block splinting and pinning
![]() Traction, dynamic or static (see Chap. HA-35).
Traction, dynamic or static (see Chap. HA-35).
![]() Unstable, irreducible fractures, typically involving more than 30% to 50% of the joint, require:
Unstable, irreducible fractures, typically involving more than 30% to 50% of the joint, require:
![]() External fixation
External fixation
![]() Percutaneous fixation
Percutaneous fixation
![]() Open reduction with internal fixation using K-wires, screws, cerclage wires
Open reduction with internal fixation using K-wires, screws, cerclage wires
![]() When dorsal fracture-dislocations are associated with bone loss or fracture comminution to such a degree that a stable reduction is unobtainable using the methods listed earlier, two salvage procedures are commonly employed.
When dorsal fracture-dislocations are associated with bone loss or fracture comminution to such a degree that a stable reduction is unobtainable using the methods listed earlier, two salvage procedures are commonly employed.
![]() Volar plate arthroplasty. The volar plate is advanced into the middle phalangeal defect, simultaneously restoring stability and resurfacing the damaged articular surface6,15 (see Chap. HA-37).
Volar plate arthroplasty. The volar plate is advanced into the middle phalangeal defect, simultaneously restoring stability and resurfacing the damaged articular surface6,15 (see Chap. HA-37).
![]() Hemi-hamate autograft reconstruction. The fractured middle phalangeal base is débrided, and the defect is replaced using a size-matched portion of the dorsal/distal hamate osteoarticular surface and secured with mini-fragment screws22 (see Chap. HA-38).
Hemi-hamate autograft reconstruction. The fractured middle phalangeal base is débrided, and the defect is replaced using a size-matched portion of the dorsal/distal hamate osteoarticular surface and secured with mini-fragment screws22 (see Chap. HA-38).
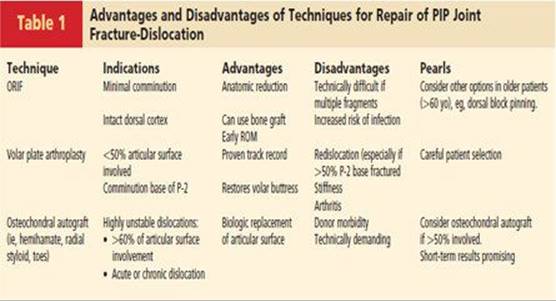
![]() Table 1 illustrates some of the indications, advantages, and disadvantages of open reduction and internal fixation and some of the salvage options discussed in this chapter.8
Table 1 illustrates some of the indications, advantages, and disadvantages of open reduction and internal fixation and some of the salvage options discussed in this chapter.8
Indications
![]() Unstable and tenuous fractures requiring more than 30 degrees of flexion to maintain reduction
Unstable and tenuous fractures requiring more than 30 degrees of flexion to maintain reduction
![]() Closed management of these fractures requires extreme flexion to prevent redislocation is likely to result in a flexion contracture.
Closed management of these fractures requires extreme flexion to prevent redislocation is likely to result in a flexion contracture.
![]() Fractures with fragments that are irreducible by closed methods and amenable to internal fixation with available hardware
Fractures with fragments that are irreducible by closed methods and amenable to internal fixation with available hardware
![]() Significant articular depression, displacement, or incongruity
Significant articular depression, displacement, or incongruity
Goals
![]() Stable, anatomic fixation of the fracture resulting in a concentric reduction of the PIP joint
Stable, anatomic fixation of the fracture resulting in a concentric reduction of the PIP joint
![]() Early range of motion designed to enhance cartilage and soft tissue healing, enhance joint remodeling, and minimize adhesions and contractures
Early range of motion designed to enhance cartilage and soft tissue healing, enhance joint remodeling, and minimize adhesions and contractures
![]() Anatomic restoration of the congruous joint surface is a desirable but less important treatment goal and does not supersede a concentric PIP reduction and early motion.
Anatomic restoration of the congruous joint surface is a desirable but less important treatment goal and does not supersede a concentric PIP reduction and early motion.
Preoperative Planning
![]() Radiographic evaluation, as discussed earlier
Radiographic evaluation, as discussed earlier
![]() The surgeon must be adept at using the various techniques, and the patient should be counseled that intraoperative observations will dictate the definitive method of fixation.
The surgeon must be adept at using the various techniques, and the patient should be counseled that intraoperative observations will dictate the definitive method of fixation.
Positioning
![]() The patient is placed supine with a radiolucent hand table.
The patient is placed supine with a radiolucent hand table.
![]() A brachial tourniquet is placed on the upper arm before draping and is inflated to 250 mm Hg just before the incision is made.
A brachial tourniquet is placed on the upper arm before draping and is inflated to 250 mm Hg just before the incision is made.
![]() Surgery can be performed under a wrist or digital block, but an axillary block is preferred to obtain adequate sensory anesthesia and motor relaxation of the flexors and extensors.
Surgery can be performed under a wrist or digital block, but an axillary block is preferred to obtain adequate sensory anesthesia and motor relaxation of the flexors and extensors.
![]() The operative hand is supinated, and a “lead hand” can be used to hold it in place.
The operative hand is supinated, and a “lead hand” can be used to hold it in place.
Operative Equipment
![]() A mini C-arm fluoroscopy unit is necessary to confirm fracture reduction, joint reduction, and correct placement of implants.
A mini C-arm fluoroscopy unit is necessary to confirm fracture reduction, joint reduction, and correct placement of implants.
![]() Mini-fragment plate and screw set
Mini-fragment plate and screw set
![]() 24-gauge wire
24-gauge wire
![]() K-wires
K-wires
Approach
![]() The volar (Bruner) approach, the dorsal (Chamay) approach, and the mid-axial approach are all useful.
The volar (Bruner) approach, the dorsal (Chamay) approach, and the mid-axial approach are all useful.
![]() The approach is chosen based on the fracture pattern and the direction of instability.
The approach is chosen based on the fracture pattern and the direction of instability.
![]() When most of the fracture comminution is dorsal, a Chamay or mid-axial approach is selected.
When most of the fracture comminution is dorsal, a Chamay or mid-axial approach is selected.
![]() When most of the comminution is volar, as is more common with dorsal fracture-dislocations, a volar Bruner incision is employed.
When most of the comminution is volar, as is more common with dorsal fracture-dislocations, a volar Bruner incision is employed.
TECHNIQUES
EXPOSURE
Volar Approach (Bruner) 3,10
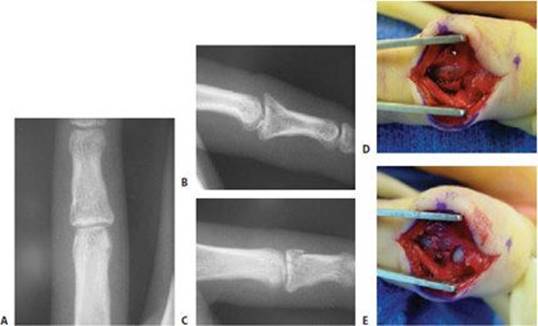
![]() A palmar zigzag skin incision is made from the MCP joint crease across the PIP joint to the DIP flexion crease. In a larger or longer digit, two limbs of a Bruner incision may be necessary between the flexion creases (TECH FIG 1A,B).
A palmar zigzag skin incision is made from the MCP joint crease across the PIP joint to the DIP flexion crease. In a larger or longer digit, two limbs of a Bruner incision may be necessary between the flexion creases (TECH FIG 1A,B).
![]() An ulnarly based, thick subcutaneous flap is mobilized at the level of the flexor sheath.
An ulnarly based, thick subcutaneous flap is mobilized at the level of the flexor sheath.
![]() The digital neurovascular structures are mobilized from the flexor sheath apparatus.
The digital neurovascular structures are mobilized from the flexor sheath apparatus.
![]() These procedures are necessary to avoid traction on the associated structures if the joint is dorsally displaced during exposure and fixation.
These procedures are necessary to avoid traction on the associated structures if the joint is dorsally displaced during exposure and fixation.
![]() The flexor sheath over the PIP joint (including the A3 pulley) is incised on three sides, creating a rectangular flap between the A2 and A4 pulleys (TECH FIG 1C).
The flexor sheath over the PIP joint (including the A3 pulley) is incised on three sides, creating a rectangular flap between the A2 and A4 pulleys (TECH FIG 1C).
![]() Alternatively, the flexor sheath may be split longitudinally to expose the underlying flexor tendons.
Alternatively, the flexor sheath may be split longitudinally to expose the underlying flexor tendons.
![]() The flexor digitorum profundus and flexor digitorum superficialis tendons are retracted to the side to expose the volar plate (TECH FIG 1D).
The flexor digitorum profundus and flexor digitorum superficialis tendons are retracted to the side to expose the volar plate (TECH FIG 1D).
![]() A Penrose drain placed around the tendons permits atraumatic retraction.
A Penrose drain placed around the tendons permits atraumatic retraction.
![]() The PIP joint and bare surface of the volar fragment are exposed by dividing the volar plate in the transverse plane just proximal to its distal insertion.
The PIP joint and bare surface of the volar fragment are exposed by dividing the volar plate in the transverse plane just proximal to its distal insertion.
![]() Make sure to leave a small amount of the distal portion attached to the bony fragment of the middle phalanx for later repair.
Make sure to leave a small amount of the distal portion attached to the bony fragment of the middle phalanx for later repair.
![]() Retract the main portion of the volar plate proximally, creating a proximally based flap. The volar plate is not excised.
Retract the main portion of the volar plate proximally, creating a proximally based flap. The volar plate is not excised.
![]() Sharp recession of the collateral ligaments at their proximal or distal volar attachments may be required to access fragments that are more dorsal than the volar third of the middle phalangeal base or to reduce chronic subluxations.
Sharp recession of the collateral ligaments at their proximal or distal volar attachments may be required to access fragments that are more dorsal than the volar third of the middle phalangeal base or to reduce chronic subluxations.
![]() Most often, the collateral ligaments are elevated only from their middle phalangeal insertion.
Most often, the collateral ligaments are elevated only from their middle phalangeal insertion.
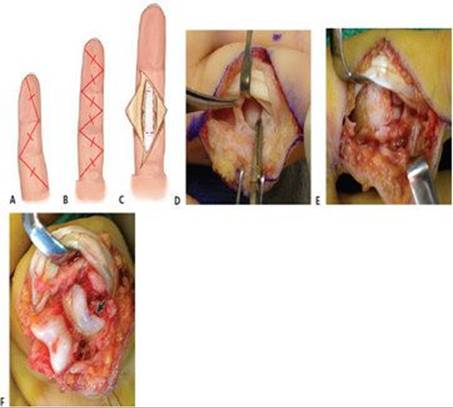
TECH FIG 1 • A. The Bruner approach uses a palmar zigzag skin incision from the metacarpophalangeal (MCP) flexion crease across the PIP joint level to the DIP flexion crease. B. In larger digits, two limbs may be necessary between flexion creases. C. Once the flexor sheath is exposed, it can be incised on three sides between the A2 and A4 pulleys and the flap retracted laterally. Alternatively, the sheath can be split down its center longitudinally to expose the flexor tendons. The pathways of the incisions are demonstrated by the dotted line. D. After retraction of the incised flexor sheath, the flexor digitorum and profundus tendons (FDP, FDS) are exposed. Gently retract them to one side with a blunt retractor to expose the volar plate and the base of the middle phalanx. Not uncommonly, the volar plate is still attached to the volar lip of the middle phalangeal fracture fragment. E,F. Shotgun exposure of the PIP joint. E. The PIP joint is distracted while the flexor tendons are retracted laterally. F. The joint is then gently hyperextended until it maintains this shotgun alignment of its own accord (˜130 degrees), exposing the articular surfaces (arrow, fractured volar middle phalanx base). (D-F: hand is to the left and the finger is to the right).
TECH FIG 2 • Dorsal (Chamay) approach. A. A longitudinal skin incision is made midline over the dorsal aspect of the proximal phalanx proximally and then is curved laterally and distally around the dorsal aspect of the PIP joint. B. After superficial dissection is carried down to expose the extensor mechanism, a distally based, V-shaped flap of central slip is created, with the apex of the flap extending to the proximal third of the proximal phalanx. This pedicle flap of central slip is then pulled distally with a hooked retractor to expose the PIP joint.
![]() If comprehensive exposure of the PIP joint is required, the collateral ligaments are released from their site of insertion, and the PIP joint is distracted and then gently hyperextended until it maintains this alignment of its own accord (about 130 degrees). This has been referred to as “shotgun” exposure of the joint6 (TECH FIG 1E,F).
If comprehensive exposure of the PIP joint is required, the collateral ligaments are released from their site of insertion, and the PIP joint is distracted and then gently hyperextended until it maintains this alignment of its own accord (about 130 degrees). This has been referred to as “shotgun” exposure of the joint6 (TECH FIG 1E,F).
![]() Watch the neurovascular bundles closely during this hyperextension maneuver to ensure they can easily subluxate dorsally.
Watch the neurovascular bundles closely during this hyperextension maneuver to ensure they can easily subluxate dorsally.
Dorsal Approach (Chamay) 4
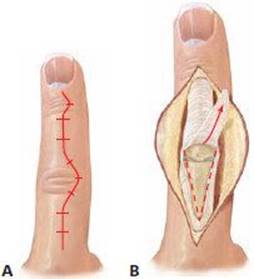
![]() A longitudinal skin incision is made over the dorsal aspect of the PIP joint along the midline proximally and distally curving around the dorsal aspect of the PIP joint, exposing the extensor mechanism (TECH FIG 2A).
A longitudinal skin incision is made over the dorsal aspect of the PIP joint along the midline proximally and distally curving around the dorsal aspect of the PIP joint, exposing the extensor mechanism (TECH FIG 2A).
![]() A distally based, V-shaped flap of central slip with the pedicle extending as far as the proximal third of the proximal phalanx is made (TECH FIG 2B).
A distally based, V-shaped flap of central slip with the pedicle extending as far as the proximal third of the proximal phalanx is made (TECH FIG 2B).
![]() The extensor flap is reflected distally, allowing the intact lateral bands to slip palmarly and laterally, providing a wide exposure of the PIP joint.
The extensor flap is reflected distally, allowing the intact lateral bands to slip palmarly and laterally, providing a wide exposure of the PIP joint.
![]() On completion of the surgery, the central slip is securely sutured in place with 4-0 nonabsorbable suture.
On completion of the surgery, the central slip is securely sutured in place with 4-0 nonabsorbable suture.
![]() The repair is strong and will allow early active motion within the first 48 hours.
The repair is strong and will allow early active motion within the first 48 hours.
TECH FIG 3 • A. Diagrams demonstrating the midaxial (blue line) and midlateral (red line) approaches. The midlateral approach is shown for reference, but the midaxial approach is the one most often used clinically. Midaxial approach (blue): flex the finger and mark the motion axes of the IP joints by marking the points at the IP joints where the flexion creases end dorsally. Draw a line through these points proximally and distally (blue line). B. In a cross-section diagram of these approaches, the midaxial dissection will be dorsal to the neurovascular bundle and the midlateral dissection will be at the level of the neurovascular bundle.
Mid-Axial Approach
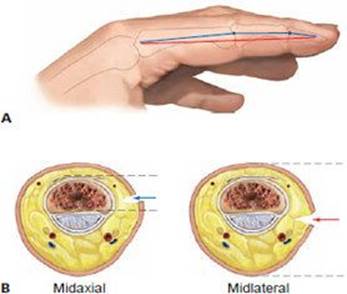
![]() Identify the midaxial line by marking the axes of the IP joints and drawing a line through these points proximally and distally (TECH FIG 3A).
Identify the midaxial line by marking the axes of the IP joints and drawing a line through these points proximally and distally (TECH FIG 3A).
![]() Make the skin incision on this midaxial line. The digital nerve and artery lie about 2 mm volar to the margin of the incision (TECH FIG 3B).
Make the skin incision on this midaxial line. The digital nerve and artery lie about 2 mm volar to the margin of the incision (TECH FIG 3B).
![]() Avoid a radial-sided incision on the index finger and an ulnar-sided incision on the small finger. These surfaces are important for contact and should be protected from potential scar sensitivity.
Avoid a radial-sided incision on the index finger and an ulnar-sided incision on the small finger. These surfaces are important for contact and should be protected from potential scar sensitivity.
![]() The first structure encountered in the subcutaneous fat is Cleland’s ligament, which contains fibers that run volar to dorsal and consist of thin fascial layers surrounding the digital nerve and artery with skin. It can be isolated from adjacent fat at the level of the PIP joint.
The first structure encountered in the subcutaneous fat is Cleland’s ligament, which contains fibers that run volar to dorsal and consist of thin fascial layers surrounding the digital nerve and artery with skin. It can be isolated from adjacent fat at the level of the PIP joint.
![]() Once Cleland’s ligament is divided, carry the dissection slightly volarward, deep to the neurovascular bundle, and expose the lateral aspect of the middle phalanx and lateral margin of the flexor sheath.
Once Cleland’s ligament is divided, carry the dissection slightly volarward, deep to the neurovascular bundle, and expose the lateral aspect of the middle phalanx and lateral margin of the flexor sheath.
![]() The neurovascular bundle remains in the volar flap.
The neurovascular bundle remains in the volar flap.
![]() Enter the joint between the volar plate and the accessory collateral ligament and inspect the joint.
Enter the joint between the volar plate and the accessory collateral ligament and inspect the joint.
![]() Additional exposure is gained by elevating the collateral ligament at the origin or the insertion.
Additional exposure is gained by elevating the collateral ligament at the origin or the insertion.
FRACTURE AND JOINT REDUCTION
![]() The joint and fractures are exposed, cleansed of hematoma, and fully evaluated.
The joint and fractures are exposed, cleansed of hematoma, and fully evaluated.
![]() If soft tissues are interposed, a fine curved hemostat or dental pick may be introduced to clear the fracture site.
If soft tissues are interposed, a fine curved hemostat or dental pick may be introduced to clear the fracture site.
![]() A dental pick or Freer elevator may be used to carefully manipulate and elevate depressed articular fragments, restoring articular congruity.
A dental pick or Freer elevator may be used to carefully manipulate and elevate depressed articular fragments, restoring articular congruity.
![]() Maintain cancellous and subchondral bone on the articular cartilage-bearing fragments.
Maintain cancellous and subchondral bone on the articular cartilage-bearing fragments.
![]() Cancellous bone grafting may be required to prevent articular surface collapse in highly comminuted fractures.
Cancellous bone grafting may be required to prevent articular surface collapse in highly comminuted fractures.
![]() Alloor autograft (often harvested from the dorsal distal radius) can be used. The graft material is packed into the metaphysis through either direct application or a cortical window.
Alloor autograft (often harvested from the dorsal distal radius) can be used. The graft material is packed into the metaphysis through either direct application or a cortical window.
![]() Small 0.045 or 0.030-inch K-wires may be used to provisionally stabilize the reduction.
Small 0.045 or 0.030-inch K-wires may be used to provisionally stabilize the reduction.
![]() Preliminary joint reduction, fracture reduction, and articular restoration are confirmed under direct vision and with fluoroscopy.
Preliminary joint reduction, fracture reduction, and articular restoration are confirmed under direct vision and with fluoroscopy.
![]() Fracture fixation may proceed through various methods, depending on fracture pattern and surgeon preference.
Fracture fixation may proceed through various methods, depending on fracture pattern and surgeon preference.
![]() Following definitive fixation, the digit is put through full ROM under fluoroscopy to ensure a stable concentric reduction has been achieved without sign of abnormal joint motion.
Following definitive fixation, the digit is put through full ROM under fluoroscopy to ensure a stable concentric reduction has been achieved without sign of abnormal joint motion.
![]() Close evaluation of lateral fluoroscopic images is critical to ensure that the PIP joint does not remain dorsally subluxated.
Close evaluation of lateral fluoroscopic images is critical to ensure that the PIP joint does not remain dorsally subluxated.
![]() If the joint is not concentrically reduced or the internal fixation of the fracture is tenuous, it may be augmented with dynamic external fixation,13 extension block pinning, or a transarticular K-wire.5
If the joint is not concentrically reduced or the internal fixation of the fracture is tenuous, it may be augmented with dynamic external fixation,13 extension block pinning, or a transarticular K-wire.5
MINI-FRAGMENT FIXATION
![]() Screw fixation, if attainable, provides excellent stability and may allow earlier ROM and improved functional restoration. This form of stabilization is indicated for larger and fewer fragments (TECH FIG 4A–D).
Screw fixation, if attainable, provides excellent stability and may allow earlier ROM and improved functional restoration. This form of stabilization is indicated for larger and fewer fragments (TECH FIG 4A–D).
![]() Be aware that these fragments are often more comminuted than believed, and screws may further comminute the bone, making ultimate fixation difficult.8
Be aware that these fragments are often more comminuted than believed, and screws may further comminute the bone, making ultimate fixation difficult.8
![]() After anatomic reduction of the fragments is achieved by careful manipulation and the fragments are stabilized with clamps or K-wires (as needed), appropriately sized screws, typically in the 1.0to 1.7-mm range, are chosen.
After anatomic reduction of the fragments is achieved by careful manipulation and the fragments are stabilized with clamps or K-wires (as needed), appropriately sized screws, typically in the 1.0to 1.7-mm range, are chosen.
![]() The screw hole is drilled as perpendicular to the fracture plane as possible.
The screw hole is drilled as perpendicular to the fracture plane as possible.
![]() The depth is measured.
The depth is measured.
![]() If possible, an interfragmentary lag technique is preferred. This is done by overdrilling the near fragment cortex with a drill equal to the screw’s outer diameter.
If possible, an interfragmentary lag technique is preferred. This is done by overdrilling the near fragment cortex with a drill equal to the screw’s outer diameter.
![]() A self-tapping, minifragment cortical screw is placed.
A self-tapping, minifragment cortical screw is placed.
![]() Countersinking of screws or use of headless screws may be helpful to avoid soft tissue tethering and tendon irritation (TECH FIG 4E).
Countersinking of screws or use of headless screws may be helpful to avoid soft tissue tethering and tendon irritation (TECH FIG 4E).
![]() If the fragment is large enough, two screws, or a screw and a supplementary threaded K-wire (0.028 inch), can be used to prevent rotation of the fragment (TECH FIG 4F,G).
If the fragment is large enough, two screws, or a screw and a supplementary threaded K-wire (0.028 inch), can be used to prevent rotation of the fragment (TECH FIG 4F,G).
![]() After the procedure, PIP joint ROM usually is compromised, with a residual flexion contracture occurring in more than 80% of cases of volar fracture and dorsal instability.11
After the procedure, PIP joint ROM usually is compromised, with a residual flexion contracture occurring in more than 80% of cases of volar fracture and dorsal instability.11

TECH FIG 4 • A–C. Preoperative AP, lateral, and oblique radiographs demonstrating a displaced small finger PIP intra-articular fracture with a large dorsal/ulnar fragment. D,E. Intraoperative photos show the dorsal approach to the PIP joint. D. The fragment was large enough to be amenable to microscrew fixation. E. Using standard AO technique, a 1.7-mm screw was placed to achieve stable fixation of the fragment. The head of the screw has been countersunk. F,G. Postoperative AP and lateral radiographs demonstrate the screw in position and a reduced joint surface.
CERCLAGE WIRE TECHNIQUE
![]() The cerclage wire technique 20 allows reduction of multiple small articular fragments and provides adequate fixation to allow early ROM exercises (TECH FIG 5A).
The cerclage wire technique 20 allows reduction of multiple small articular fragments and provides adequate fixation to allow early ROM exercises (TECH FIG 5A).
![]() A thorough joint release is required, which carries the risk of increased fibrosis and stiffness postoperatively.
A thorough joint release is required, which carries the risk of increased fibrosis and stiffness postoperatively.
![]() A volar incision with a “shotgun” exposure of the PIP joint is used (TECH FIG 5B).
A volar incision with a “shotgun” exposure of the PIP joint is used (TECH FIG 5B).
![]() Judicious elevation of the central slip is performed.
Judicious elevation of the central slip is performed.
![]() A thin ring of periosteum around the bony fragments of the middle phalanx is cleared by sharp dissection.
A thin ring of periosteum around the bony fragments of the middle phalanx is cleared by sharp dissection.
![]() This allows the wire loop to seat directly against bone, providing firm fixation of the fracture fragments.
This allows the wire loop to seat directly against bone, providing firm fixation of the fracture fragments.
![]() The normal shape of the base of the middle phalanx (reverse funnel contour) also aids in fixation of the wire and prevents postoperative slippage, even with early ROM.
The normal shape of the base of the middle phalanx (reverse funnel contour) also aids in fixation of the wire and prevents postoperative slippage, even with early ROM.
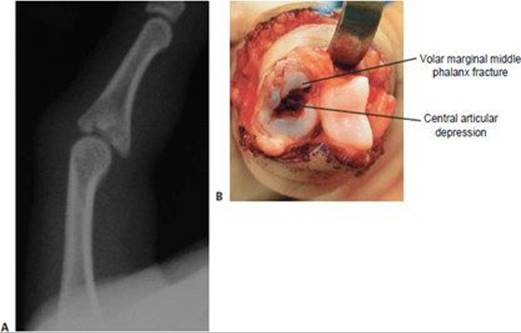
TECH FIG 5 • Cerclage wire technique. A. Lateral radiograph demonstrates a pilon-type fracture pattern of the middle phalanx, with depressed central articular fragments. B. After “shotgun” exposure, central articular impaction is evident in addition to marginal comminution. This fracture is a good candidate for cerclage wiring, because this pattern would be difficult to reduce and maintain with screw or K-wire fixation. (continued)
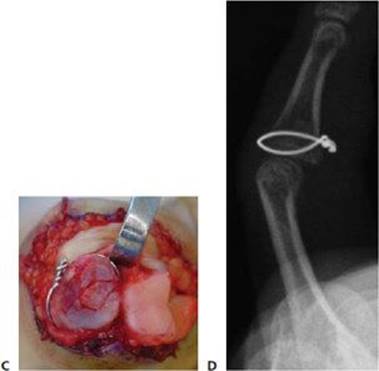
TECH FIG 5 • (continued) C. The central fragment has been reduced and a 24-gauge steel wire was formed into a loop and gently placed, allowing circumferential compression of the fracture fragments. D.A postoperative lateral radiograph confirms correction of the central articular depression.
![]() 24-gauge steel wire is formed into a loop and twisted on itself until the loop is partially closed, just larger than the base of the middle phalanx.
24-gauge steel wire is formed into a loop and twisted on itself until the loop is partially closed, just larger than the base of the middle phalanx.
![]() After fracture reduction, the loop of wire is seated and gently tightened, allowing circumferential compression of the fracture fragments (TECH FIG 5C).
After fracture reduction, the loop of wire is seated and gently tightened, allowing circumferential compression of the fracture fragments (TECH FIG 5C).
![]() Final confirmation of articular reduction is made, with careful attention to the correction of central depression and joint subluxation (TECH FIG 5D).
Final confirmation of articular reduction is made, with careful attention to the correction of central depression and joint subluxation (TECH FIG 5D).
![]() The twisted portion of the loop is placed on the volar or volar lateral surface or the middle phalanx base, flush to the cortex, at the edge of the volar plate.
The twisted portion of the loop is placed on the volar or volar lateral surface or the middle phalanx base, flush to the cortex, at the edge of the volar plate.
![]() The wire is covered by the repaired volar plate to prevent mechanical irritation of the flexor tendons.
The wire is covered by the repaired volar plate to prevent mechanical irritation of the flexor tendons.
Supplementary K-Wire Addition
![]() A supplementary K-wire may be necessary, depending on fracture configuration (TECH FIG 6A,B).
A supplementary K-wire may be necessary, depending on fracture configuration (TECH FIG 6A,B).
![]() The cerclage wire is loosely twisted around the base of the middle phalanx, maintaining the position of the articular fragments prior to the replacement of the central and volar depressed fragment (TECH FIG 6C).
The cerclage wire is loosely twisted around the base of the middle phalanx, maintaining the position of the articular fragments prior to the replacement of the central and volar depressed fragment (TECH FIG 6C).
![]() After replacement of the central fragment and further fixation with a K-wire, the cerclage wire is tightened (TECH FIG 6D,E) and the tail cut.
After replacement of the central fragment and further fixation with a K-wire, the cerclage wire is tightened (TECH FIG 6D,E) and the tail cut.
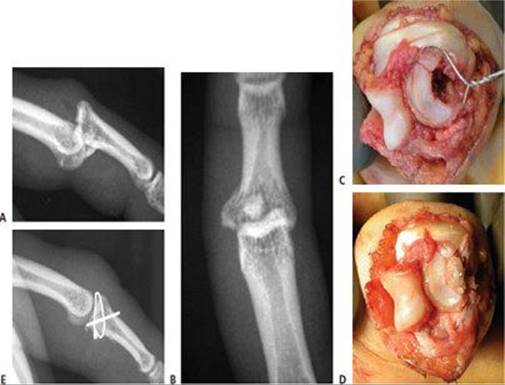
TECH FIG 6 • Cerclage wire technique with K-wire supplementation. A,B. Preoperative lateral and AP injury radiographs demonstrating a dorsal fracture-dislocation with central and volar articular depression and comminution. C. The cerclage wire is twisted loosely to around the base of the middle phalanx, maintaining the position of the articular fragments before reduction of the central and volar depressed fragment. D. After reduction of the central fragment and further fixation with a K-wire, the cerclage wire is tightened. The “tail” is then turned 90 degrees so that it is flush with the bone and cut. E.A postoperative lateral radiograph demonstrates restoration of the articular surface and reduction of the dislocation.
CLOSURE AND SPLINTING
![]() The volar plate and central slip flaps are closed with a 4-0 nonabsorbable suture.
The volar plate and central slip flaps are closed with a 4-0 nonabsorbable suture.
![]() The flexor tendon sheath is closed using either absorbable or nonabsorbable 5-0 or 6-0 suture.
The flexor tendon sheath is closed using either absorbable or nonabsorbable 5-0 or 6-0 suture.
![]() The tourniquet is deflated, and hemostasis is achieved with bipolar cautery.
The tourniquet is deflated, and hemostasis is achieved with bipolar cautery.
![]() The skin is closed with 5-0 nylon suture.
The skin is closed with 5-0 nylon suture.
![]() The patient is placed into an intrinsic-plus volar splint. Usually, the MP joints are flexed 70 to 90 degrees and the IP joints are extended based on the stability of fixation and joint reduction.
The patient is placed into an intrinsic-plus volar splint. Usually, the MP joints are flexed 70 to 90 degrees and the IP joints are extended based on the stability of fixation and joint reduction.
POSTOPERATIVE CARE
![]() Progressive active and active assisted range of motion does not begin until postoperative day 2 to 5, depending on initial patient comfort.
Progressive active and active assisted range of motion does not begin until postoperative day 2 to 5, depending on initial patient comfort.
![]() A thermoplastic splint provides protected mobilization.
A thermoplastic splint provides protected mobilization.
![]() Relatively more aggressive flexion than extension (less than 30 degrees) is pursued with the therapist.
Relatively more aggressive flexion than extension (less than 30 degrees) is pursued with the therapist.
![]() Close weekly follow-up for the first 3 weeks is necessary to monitor for any loss of reduction.
Close weekly follow-up for the first 3 weeks is necessary to monitor for any loss of reduction.
![]() All restrictions on motion are removed at 5 to 6 weeks, and radiographic signs of healing are followed.
All restrictions on motion are removed at 5 to 6 weeks, and radiographic signs of healing are followed.
![]() Therapy is continued for 1 to 2 months after removal of the splint, to recover motion and strengthen the hand.
Therapy is continued for 1 to 2 months after removal of the splint, to recover motion and strengthen the hand.
OUTCOMES
![]() Green and Akelman reported on two patients with dorsal fracture-dislocations who underwent ORIF and reported an average active range of motion of 95 degrees at 1-year follow-up, with neither patient demonstrating any evidence of subluxation.10,13
Green and Akelman reported on two patients with dorsal fracture-dislocations who underwent ORIF and reported an average active range of motion of 95 degrees at 1-year follow-up, with neither patient demonstrating any evidence of subluxation.10,13
![]() Hastings and Carroll12 reported on 15 patients treated with ORIF using various combinations of K-wire fixation, tension band wire fixation, and screw fixation. Eventual average postoperative ROM was 17 to 90 degrees.
Hastings and Carroll12 reported on 15 patients treated with ORIF using various combinations of K-wire fixation, tension band wire fixation, and screw fixation. Eventual average postoperative ROM was 17 to 90 degrees.
![]() Dietch et al5 reported on 24 patients with unstable dorsal fracture dislocations of the PIP joint treated with two methods, volar plate arthroplasty and ORIF. At an average follow-up of 46 months, results indicated that if reduction of the joint is maintained, patients could expect few functional deficits despite radiographic degenerative changes and loss of mobility.
Dietch et al5 reported on 24 patients with unstable dorsal fracture dislocations of the PIP joint treated with two methods, volar plate arthroplasty and ORIF. At an average follow-up of 46 months, results indicated that if reduction of the joint is maintained, patients could expect few functional deficits despite radiographic degenerative changes and loss of mobility.
![]() Weiss20 reported on 12 patients with dorsal fracturedislocations treated with cerclage wire fixation and reported an average ROM of 89 degrees at 2 years follow-up, with no complications and only one patient with evidence of radiographic degenerative changes.
Weiss20 reported on 12 patients with dorsal fracturedislocations treated with cerclage wire fixation and reported an average ROM of 89 degrees at 2 years follow-up, with no complications and only one patient with evidence of radiographic degenerative changes.
![]() Stern et al19 reported on 20 patients with pilon fracturedislocations of the PIP joint. They used three treatment methods: splinting, skeletal traction, and open reduction with K-wire fixation. After a clinical and radiographic follow-up of 25 months, skeletal traction led to fewer complications and clinically comparable outcomes to open reduction (achieving an average ROM of 80 degrees vs. 70 degrees, respectively).
Stern et al19 reported on 20 patients with pilon fracturedislocations of the PIP joint. They used three treatment methods: splinting, skeletal traction, and open reduction with K-wire fixation. After a clinical and radiographic follow-up of 25 months, skeletal traction led to fewer complications and clinically comparable outcomes to open reduction (achieving an average ROM of 80 degrees vs. 70 degrees, respectively).
![]() While clinical experience supports anatomic reduction of intra-articular fractures in weight-bearing joints such as the hip or knee, most laboratory and clinical reports support the theory that anatomic surface restoration is unnecessary if subluxation is corrected and motion is instituted shortly after injury.1,11, 17
While clinical experience supports anatomic reduction of intra-articular fractures in weight-bearing joints such as the hip or knee, most laboratory and clinical reports support the theory that anatomic surface restoration is unnecessary if subluxation is corrected and motion is instituted shortly after injury.1,11, 17
COMPLICATIONS
![]() Degenerative arthritis
Degenerative arthritis
![]() Loss of PIP joint motion, stiffness, flexion contracture, and extensor lag
Loss of PIP joint motion, stiffness, flexion contracture, and extensor lag
![]() Loss of fixation or redisplacement
Loss of fixation or redisplacement
![]() Persistent subluxation or dislocation
Persistent subluxation or dislocation
![]() Infection
Infection
![]() Malunion
Malunion
![]() Boutonnière deformity
Boutonnière deformity
![]() Pain
Pain
REFERENCES
1. Agee JM. Unstable fracture dislocations of the proximal interphalangeal joint. Treatment with the force couple splint. Clin Orthop Relat Res 1987;214:101–112.
2. Blazar PE, Steinberg DR. Fractures of the proximal interphalangeal joint. J Am Acad Orthop Surg 2000;8:383–390.
3. Bruner JM. Surgical exposure of the flexor tendons in the hand. Ann R Coll Surg Engl 1973;53:84–94.
4. Chamay A. A distally based dorsal and triangular tendinous flap for direct access to proximal interphalangeal joint. Ann Chir Main 1988;7:179–183.
5. Deitch MA, Kiefhaber TR, Stern PJ. Dorsal fracture dislocations of the proximal interphalangeal joint: surgical complications and longterm results. J Hand Surg Am 1999;24:914–923.
6. Eaton RG, Malerich MM. Volar plate arthroplasty for the proximal interphalangeal joint: A review of ten years’ experience. J Hand Surg Am 1980;5:260–268.
7. Elson RA. Rupture of the central slip of the extensor hood of the finger. A test for early diagnosis. J Bone Joint Surg Br 1986;68B:229–231.
8. Freeland AE, Benoist LA. Open reduction and internal fixation method for fractures at the proximal interphalangeal joint. Hand Clin 1994;10:239–250.
9. Glickel SZ, Barron OA. Proximal interphalangeal joint fracture dislocations. Hand Clinics 2000;16:333–344.
10. Green A, Akelman E, et al. Acute open reduction and rigid internal fixation of proximal interphalangeal joint fracture dislocation. J Hand Surg Am 1992;17:512–517.
11. Hamilton SC, Stern PJ, Fassler PR, et al. Mini-screw fixation of proximal interphalangeal joint dorsal fracture-dislocations. J Hand Surg Am 2006;31:1349–1354.
12. Hastings H, Carroll C. Treatment of closed articular fractures of the metacarpophalangeal and proximal interphalangeal joints. Hand Clin 1999;6:429–453.
13. Kiefhaber TR, Stern PJ. Fracture dislocations of the proximal interphalangeal joint. J Hand Surg Am 1998;23:368–380.
14. Kiefhaber TR, Stern PJ, Grood ES. Lateral stability of the proximal interphalangeal joint. J Hand Surg Am 1986;11:661–669.
15. Malerich MM, Eaton RG. The volar plate reconstruction for fracture-dislocation of the proximal interphalangeal joint. Hand Clin 1994;10:251–260.
16. McCue FC, Honner R, Johnson MC, et al. Athletic injuries of the proximal interphalangeal joint requiring surgical treatment. J Bone Joint Surg Am 1970;52A:937–956.
17. Morgan JP, et. al. Dynamic digital traction for unstable comminuted intraarticular fracture-dislocations of the proximal interphalangeal joint. J Hand Surg Am 1995;20:565–573.
18. Schenck RR. Dynamic traction and early passive movement for fractures of the proximal interphalangeal joint. J Hand Surg Am 1986;11:850–858.
19. Stern PJ, Roman RJ, Kiefhaber TR, et al. Pilon fractures of the proximal interphalangeal joint. J Hand Surg Am 1991;16: 844–850.
20. Weiss AP. Cerclage fixation for fracture dislocation of the proximal interphalangeal joint. Clin Orthop Relat Res 1996;327:21–28.
21. Weiss AP, Hastings H 2nd. Distal unicondylar fractures of the proximal phalanx. J Hand Surg Am 1993;18:594–599.
22. Williams RM, Kiefhaber TR, Sommerkamp TG, et al. Treatment of unstable dorsal proximal interphalangeal fracture/dislocations using hemi-hamate autograft. J Hand Surg Am 2003;28:856–865.
23. Wolfe SW, Katz LD. Intra-articular impaction fractures of the phalanges. J Hand Surg Am 1995;20:327–333.